MEDICAL CODING AND BILLING
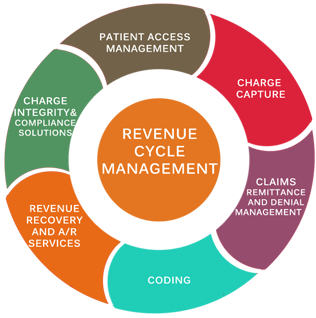 Max Trans is one of the leading Medical Billing outsourcing company offering high quality services to the clients. We successfully translate our quality and productivity into accuracy and reliability in medical claim management. We offer a completely integrated workflow to our clients, so as to eliminate the unnecessary delays and the claim denials. We understand the effect of timely claim processing on the whole healthcare revenue cycle and thus strive to provide accurate and faster service, so as to result in faster billing, faster reimbursement and improved cash flow.
Max Trans is one of the leading Medical Billing outsourcing company offering high quality services to the clients. We successfully translate our quality and productivity into accuracy and reliability in medical claim management. We offer a completely integrated workflow to our clients, so as to eliminate the unnecessary delays and the claim denials. We understand the effect of timely claim processing on the whole healthcare revenue cycle and thus strive to provide accurate and faster service, so as to result in faster billing, faster reimbursement and improved cash flow.
Our dedicated group of medical billing professionals have proven expertise in handling the different medical specialties. All our medical billing services are in full compliance with the HIPAA regulations. Our professionals have medical billing expertise in different specialties such as Radiology, Pathology, Internal medicine, Urology, Orthopedics, Gastroenterology, Cardiology, Anesthesia, Psychiatric and more. We make use of the advanced medical billing software tools so as to cater to all types of complex billing needs of our clients.
Procedure we follow
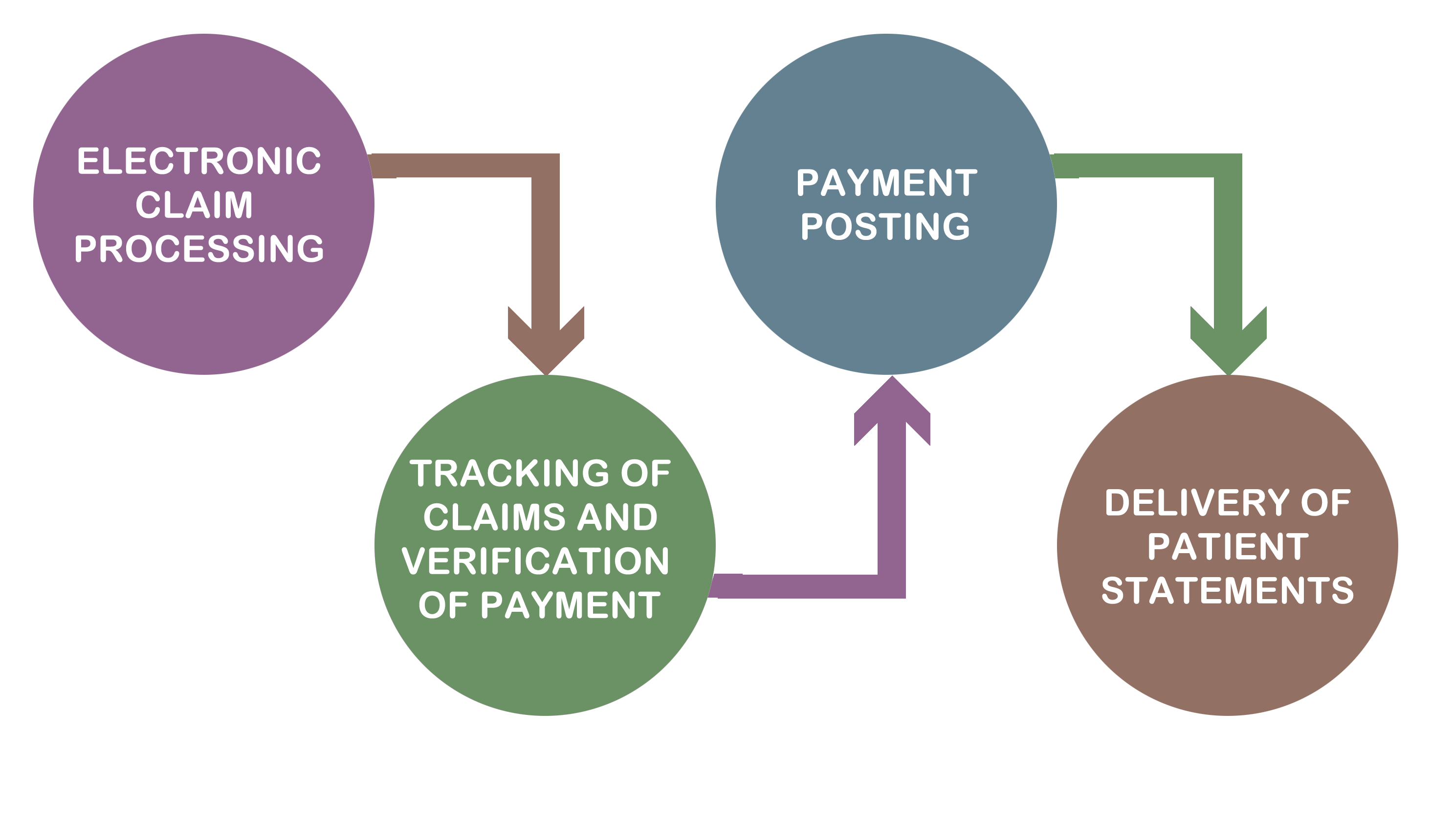
At MAX – TRANS We follow a specific set of steps to execute the medical billing services, which are as follow:
- Electronic claim processing : In this step, our professionals submit all the claims with the specific diagnostic reports and procedure codes to the insurance companies. Our quality analyst team effectively verifies all the electronic claims transfer.
- Tracking of claims and verification of payments : We execute a consistent follow-up with the insurance specialists for the accurate placement of the CPT codes and payment verification.
- Payment posting : In this step, we generate the monthly updated financial management reports.
- Delivery of the patient statements : We finally deliver the patients with their respective monthly bill statements.
Medical Billing Services
- Review of claims before submission and Review Log maintenance
- Filing of the processed claims with the insurance company
- Check for errors of coding and billing
- Receive denied claims and ensure successful reimbursement
- Generation of regular MIS claim statements
- Maintenance of Up-to-date error log